Healthcare is a huge industry, and it collects and processes an increasing amount of patient data day by day. How do organizations handle this much data? Is it possible to consolidate all data through healthcare data integration?
In this article, we’ll discuss what healthcare data integration is, and why it matters to the healthcare industry. We’ll also discuss the challenges to data integration and the best use cases for it in the world of medical organizations and patients. By the end, we’ll offer a solution that will be useful for you if you’re looking for a solid partner in data integration.
What is Healthcare Data Integration
Healthcare data integration combines data from multiple sources and turns them into a unified set.
Data can only be useful if it’s structured and easily accessible. This helps streamline the workflows of medical professionals and allows for better reporting and analytics. The main sources of information are EHRs and medical devices, but data may also come from secondary sources such as:
- Telemedicine and insurance systems
- Patient portals
- Social media
- Pharmacy management systems
The goal is to give medical professionals a broader look at patients’ health. This enables them to provide better overall healthcare services.
Benefits of Healthcare Data Integration
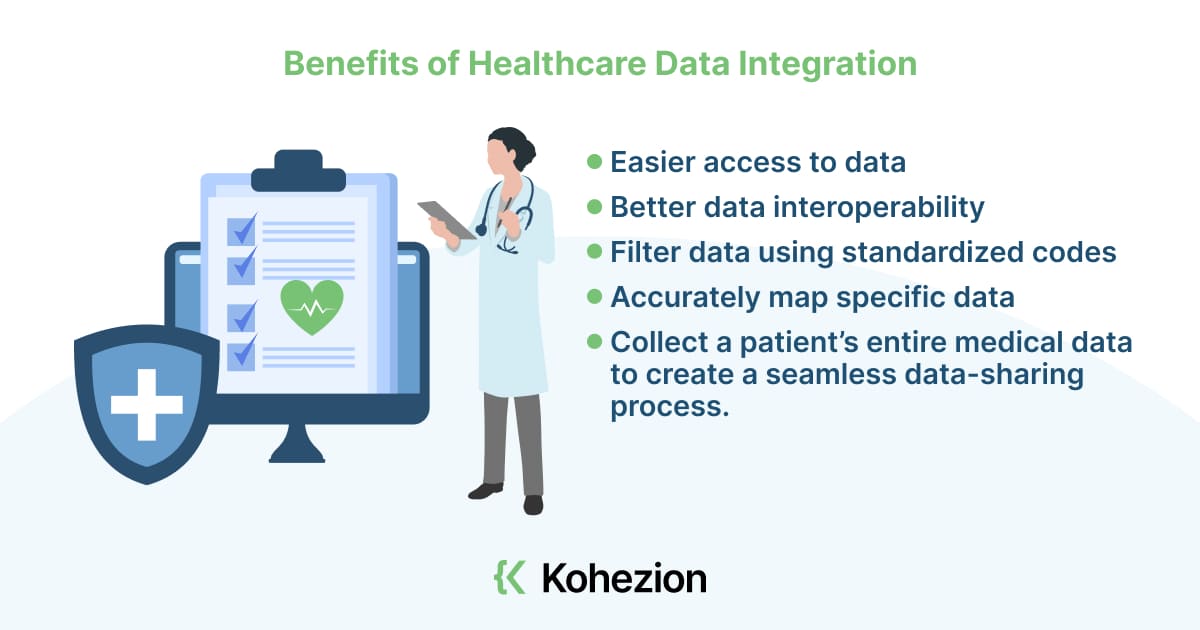
Healthcare data integration offers a ton of benefits for medical professionals and patients. Its two main benefits are:
- Easier access to data: data integration in healthcare gives hospitals better access to patient data. They can see and use the patient’s history to speed up their services, improve patient care, and reduce costs.
- Better data interoperability: interoperability is the ability of systems and software programs to communicate and exchange data. It’s also about passing through the data into a comprehensive and user-friendly interface.
Proper healthcare data access and interoperability also allow medical professionals to:
- Filter data using standardized codes, allowing them to do standardized tests, panels, and assessments.
- Accurately map specific data.
- Collect a patient’s entire medical data to create a seamless data-sharing process.
Medical Data Integration Challenges
Integrating multiple data sources into a single one isn’t a walk in the park. The healthcare IT environment is complicated. For instance, a single clinic or hospital may use a plethora of solutions to collect, store, and analyze data. The following are some of the biggest challenges to medical data integration.
Lack of Standardization
Medical data comes in different formats, and this affects data integration and usability. These sources cannot “talk” to each other or other data sources without a unified solution, leading to issues in data quality.
At the moment, no single data-formatting standard is being followed. This makes data storage and collection complicated. Subsequently, it makes data analysis and integration even more complex.
Because of this, medical professionals also struggle to automate their workflows, keep up with the changing marketplace, and offer useful data to decision-makers. Inaccurate insights, system failures, and duplicate records also happen — all of which can severely affect the quality of patient care.
Data Silos
Interoperability is hard to achieve when data silos exist. These are isolated systems that don’t operate with each other. They’re fragmented, so there’s a lack of coordination and communication.
Medical professionals may be using EHR systems that can’t operate together. They may also be using systems that struggle to integrate with new cloud-based systems. Both of these make data integration and real-time data sharing even more challenging.
This then can lead to unwanted scenarios such as duplicate data entries, inconsistent diagnoses, and inaccurate medications.
Data Security Concerns
As a highly sensitive type of information, patient data needs protection from malicious access. This becomes an even more pressing concern when data is shared between systems — it becomes a target for hackers and other cybercriminals.
There lies the two-pronged data security problem: healthcare data should be free from unauthorized access while being easily accessible to medical professionals
Also, laws such as HIPAA have compelled companies to implement separate processes for research, EMR, and billing. This brings us back to data silos and fragmented systems, making data integration even more difficult to do.
Given that, data integration must be done with a robust data governance program in place. Administrators should only have access to data at certain points in time and when certain conditions are met.
Data Application Inconsistency
The same healthcare data type can exist in two separate applications but remain inaccessible for cross-platform use. The reason: service providers use a number of applications that may or may not be compatible with each other.
Even if the data pieces are comparable, the slightest discrepancy can result in inaccurate data insights or findings. This may lead to even worse scenarios, such as misdiagnoses or ineffective medical treatments.
Best Practices for Healthcare Data Integration
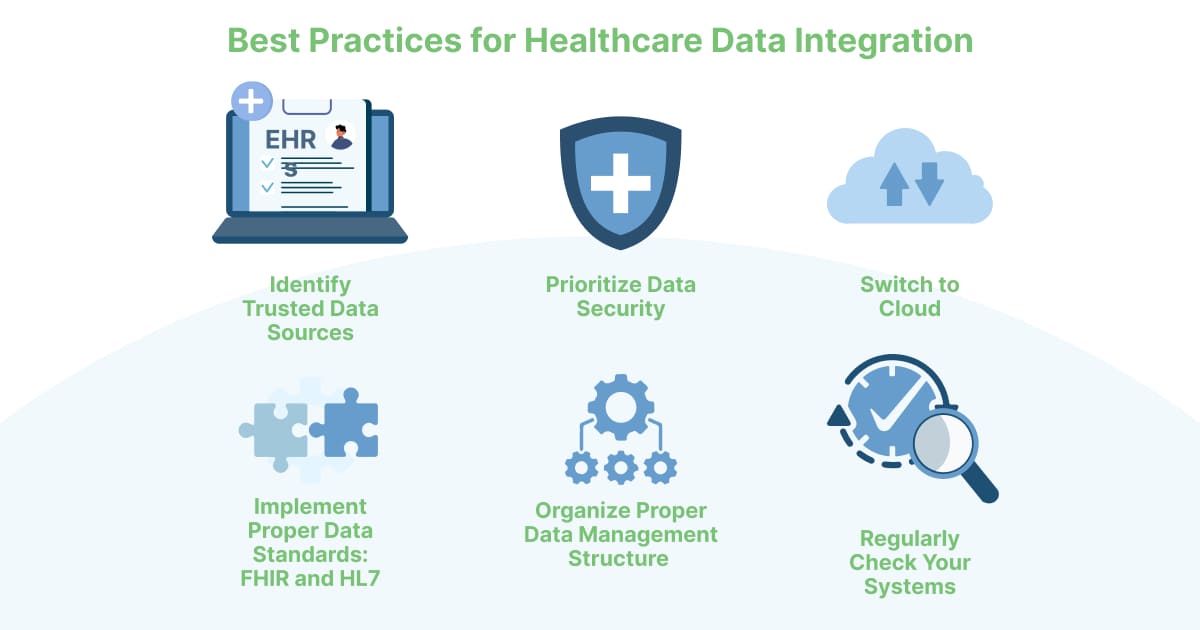
For successful healthcare data integration to happen, follow these best practices:
Identify Trusted Data Sources
Know where your required data is. Healthcare data mainly resides in EHRs, but you can also find them in other internal or external sources. Identify these sources and document them as effectively as possible.
While you’re at it, consider the types of data worth collecting. How is the information going to be used? Which program will handle it? How often should you update or maintain it? These questions will help set the boundaries for your data integration process and improve the quality of data you collect.
As you redesign your system for said data collection, consider these questions:
- What EHR system do you use, and does it cover everything you need?
- What do you need that the system doesn’t offer?
- What are your goals in using your healthcare system? Goals can be to improve the quality of patient care, reduce operational costs, or improve medical equipment usage.
Answering these questions helps guide your healthcare data integration efforts.
Prioritize Data Security
The importance of data security in healthcare can’t be overstated. Sharing medical data among service providers is a must, but it’s also extremely risky.
Implement robust security protocols and facilitate regular audits to ensure you’re protecting data. Be compliant with relevant data privacy laws and regulations such as HIPAA and GDPR.
Switch to Cloud
Switching to the cloud means achieving scalability while taking advantage of immense storage power. Not only is the cloud able to handle the sheer volume of data you require, but it’s also more cost-effective than using on-premise data centers.
Cloud computing enables real-time communication between systems. This gives medical professionals better-unified and high-quality data for decision-making.
Since medical data is distributed across vast geographical areas, you must also use API-enable architectures. They standardize data connection, resolving the issue of data fragmentation and data silos.
Implement Proper Data Standards: FHIR and HL7
FHIR (Fast Healthcare Interoperability Resources) and Health Level Seven International (HL7) are industry standards that you can use to facilitate clinical data integration.
For example, organizing your data into FHIR and HL7 formats allows you to join disparate systems. It’s a great protocol created to handle data complexity and sensitivity. It also defines how you can use APIs.
In other words, these data standards serve as the common language that enables data exchange. This way, healthcare organizations and medical professionals can share patient data with ease.
Organize Proper Data Management Structure
Data management structures refer to data lakes and data warehouses. These repositories can store and centralize data to help users run queries, create reports, perform analyses, and retrieve data.
But they also have differences:
- Data warehouses: these repositories cleanse and store structured data in relational databases. They’re ideal for generating business intelligence and painting a picture of changes data in over time. Popular examples include Microsoft Azure and Amazon Redshift.
- Data lakes: these repositories store both structured and unstructured data. They’re perfect for business analytics — you’ll understand the reasons behind past and present trends.
Apart from storing data, these data management systems can give access to the right people at the right time. Authorized people can have instant access to them, allowing for easy and smooth communication.
Regularly Check Your Systems
Checking your systems can be automated, but also perform tasks manually. This ensures you don’t miss out on anything. On top of that, you stay up to date with the latest compliance regulations and best practices.
To do this with relative ease, connect your data with available analytics tools. Ensure that database connections are secure and scalable. Doing all of these mitigates the chances of future security risks.
Healthcare Data Integration Use Cases
Healthcare data integration has many use cases for medical professionals and patients.
Response to COVID-19 Pandemic
Crisis response is a vital function of healthcare data integration. One great example is the COVID-19 pandemic, where medical professionals and the global healthcare system were tested to their limits.
Integrated healthcare data allows medical organizations to create appropriate crisis-response actions. This leads to better medical outcomes and improved care for patients. At the same time, frontliners become more well-equipped to deal with hands-on situations with patients.
Unfortunately, during the pandemic, many leaders and medical organizations didn’t have enough access to integrated data. This prevented them from making proactive decisions. The data they had was disjointed, resulting in some unpleasant situations.
Providing wider access to consolidated data could’ve made a difference. Leaders and decision-makers will have access to accurate data, allowing them to make truly informed decisions about patient care and responses to outbreaks. They can distribute vaccines effectively and coordinate with ground-level organizations to handle critical situations effectively.
Fraud Detection
Sadly, fraud is common in the healthcare industry. Identity theft is a common example, but there are also others such as overbilling and filing claims for services that have not been received. Healthcare data integration can help organizations find and prevent fraud, whether on the patient, service, or insurance level.
With consolidated data, medical organizations can cross-reference patient information, medical records, and billing records. This will allow them to find inconsistencies or irregularities, at which point they can raise alarms. Real-time monitoring, pattern recognition, identity verification, and geographic analysis are also possible.
Integrated data can also be shared with law enforcement agencies and other stakeholders. This paves the way for more effective prevention and prosecution of healthcare fraud.
As a plus, medical organizations can develop predictive models that use integrated data to automatically assess the possibility of fraudulent activities. AI and machine-learning algorithms can be applied to the models, too.
Population Health Management
Healthcare data integration is also crucial to population health management. Widespread access to data allows medical organizations to form a singular strategy for managing healthcare-related situations.
Taking the example of the COVID-19 pandemic, health professionals used data from various sources to optimize their responses to the influx of patients suffering from COVID-19 or having symptoms similar to it. One result of this was the rise of telehealth, which enabled professionals to reach patients as efficiently as possible given the circumstances.
Another example is the detection of at-risk individuals. Integrated healthcare data allows organizations to find and intervene with said at-risk individuals. Subsequently, medical departments can coordinate more effectively — duplicate tests are reduced, and patient healthcare improves.
Get Help From A Professional Healthcare Data Integration Company
Working with a professional in healthcare data integration will help you improve your efficiency, accuracy, and decision-making. Kohezion, for instance, has in-depth knowledge of designing, implementing, and maintaining data workflows.
Time-saving, scalability, customization, and data security are among the other benefits of working with Kohezion. Well-designed workflows minimize the time and effort you need to collect and analyze data. They can also handle increasing data volumes and complexity as your business grows.
Kohezion and the team behind it are also well-versed in data security and compliance. They can design systems with integrated data features while observing data-handling processes that comply with regulations.
Automate Your Healthcare Data with Kohezion
Overall, medical professionals and organizations benefit significantly from healthcare data integration. While the lack of standardization and other issues prevent many from maximizing the potential of data integration, its use cases are worth it. You can use the above best practices to enjoy those benefits and improve your healthcare data management.
Looking for a partner in healthcare data integration? Request a data health audit or try Kohezion, a highly customizable drag-and-drop online database builder that empowers you to create custom apps for data that doesn’t fit within traditional spreadsheet rows and columns.
Start building with a free account
Frequently Asked Questions
Data integration in healthcare involves the consolidation of data from various sources into a single, coherent dataset.
It aims to collect information from various sources, such as Electronic Health Records (EHRs), medical devices, telemedicine systems, pharmacy management systems, patient portals, and even social media.
The goal of healthcare data integration is to provide medical professionals with a comprehensive view of a patient's health, promoting better decision-making, patient care, and operational efficiency.
.
Data integration in healthcare enhances patient care, as it provides a complete view of medical histories. It also streamlines workflows, reduces operational costs, and improves efficiency.
Interoperability is a key benefit, allowing seamless data exchange among healthcare systems. This ensures better collaboration. At the same time, standarized coding enhances data quality.
It also enforces data security and compliance with privacy regulations like HIPAA and GDPR, safeguarding patient information. It plays a vital role in population health management, identification of at-risk individuals, and efficient resource allocation.
One example of data integration in healthcare is the integration of Electronic Health Records (EHRs) from different healthcare facilities. In many cases, patients receive care from various providers, each with their own EHR system. With data integration, these disparate systems communicate and share patient information securely.
Consider a patient who visits their primary care physician and is then referred to a specialist at a different hospital. Data integration gives the specialist access to the patient's medical history, test results, and treatment plans from the primary care physician's EHR. This exchange of data ensures that the specialist has a comprehensive understanding of the patient's health, leading to more informed decisions and better care coordination.